Antibiotic Resistance Explained: Impact, Causes, and Ways to Combat It
Discover the causes and impacts of antibiotic misuse and resistance, a growing global health crisis. Learn how misuse leads to drug-resistant bacteria and explore effective solutions to combat this threat.
Antibiotics have been one of the most significant medical advancements in human history. They have revolutionized the treatment of bacterial infections and saved countless lives. However, the misuse and overuse of antibiotics have led to a dangerous global health crisis: antibiotic resistance. This phenomenon is when bacteria evolve to resist the effects of drugs that once killed them. As a result, common infections and diseases that were once treatable have become harder to manage, leading to prolonged illness, higher medical costs, and an increased risk of death.
In this article, we will explore what antibiotic resistance is, how it develops, its implications for human health, and what can be done to address this growing issue.
What is an Antibiotic?
An antibiotic is a powerful medication used to treat bacterial infections by killing bacteria or inhibiting their growth. Antibiotics do not work against viruses, such as those causing the flu or common cold, making them specific to bacterial illnesses. These medicines have revolutionized modern healthcare, helping to treat a variety of bacterial diseases, from mild infections to severe conditions like pneumonia, tuberculosis, and urinary tract infections.
Antibiotics work through different mechanisms to combat bacteria. Some antibiotics are bactericidal, meaning they kill bacteria directly, while others are bacteriostatic, which means they inhibit the growth and reproduction of bacteria, allowing the body's immune system to eliminate the bacteria naturally. For example, Penicillin, a widely known antibiotic, prevents bacteria from forming their cell walls, causing them to burst and die. On the other hand, antibiotics like Tetracycline interfere with protein production in bacteria, preventing them from growing and multiplying.
The effectiveness of antibiotics is based on their ability to target specific parts of bacterial cells that are not present in human cells. This makes them highly effective at treating infections without harming the body's healthy tissues.
However, the overuse and misuse of antibiotics have become a global concern, leading to antibiotic resistance, where bacteria evolve to become resistant to the drugs designed to kill them. This growing problem makes it harder to treat infections, underlining the importance of using antibiotics only when necessary and as prescribed by healthcare professionals.
What is Antibiotic Misuse?
Antibiotic misuse refers to the inappropriate or incorrect use of antibiotics, which can contribute to the development of antibiotic resistance and decrease the effectiveness of these life-saving drugs. Misusing antibiotics can occur in various ways, including taking them without a prescription, not following the prescribed dosage, or using them for conditions that don’t require them, such as viral infections.
Here are some common examples of antibiotic misuse:
1. Taking antibiotics without a prescription: Often, individuals may self-medicate with antibiotics to treat an illness, even without consulting a doctor. This is dangerous, as it may not be the right treatment for the infection, and the incorrect antibiotic or dosage may cause side effects or resistance.
2. Not completing the full course: Sometimes, people stop taking antibiotics once they start feeling better, thinking the infection is gone. However, not completing the prescribed course allows some bacteria to survive, potentially leading to a relapse or the development of resistant strains.
3. Using antibiotics for viral infections: Antibiotics are ineffective against viral infections like the flu, the common cold, or COVID-19. Using them in such cases not only wastes the medication but also promotes unnecessary resistance, making it harder to treat bacterial infections in the future.
4. Taking antibiotics for non-bacterial conditions: Misusing antibiotics can also occur when they are used for conditions where they aren't needed, such as for minor illnesses or preventative purposes without any confirmed bacterial infection.
These forms of misuse can contribute significantly to the growing global problem of antibiotic resistance, where bacteria evolve to survive even the strongest antibiotics, rendering them ineffective for treating future infections.
Harmful Effects of Antibiotic Misuse: A Threat to Human Civilization
The misuse of antibiotics poses significant risks to human health and represents an emerging global threat to civilization. One of the most concerning consequences is the development of antibiotic resistance. When antibiotics are overused or misused, bacteria can develop resistance to these medications, rendering them ineffective in treating infections. This is a threat to public health, as it limits treatment options and leads to more severe infections that are harder to manage.
Antibiotic Resistance: The Growing Threat
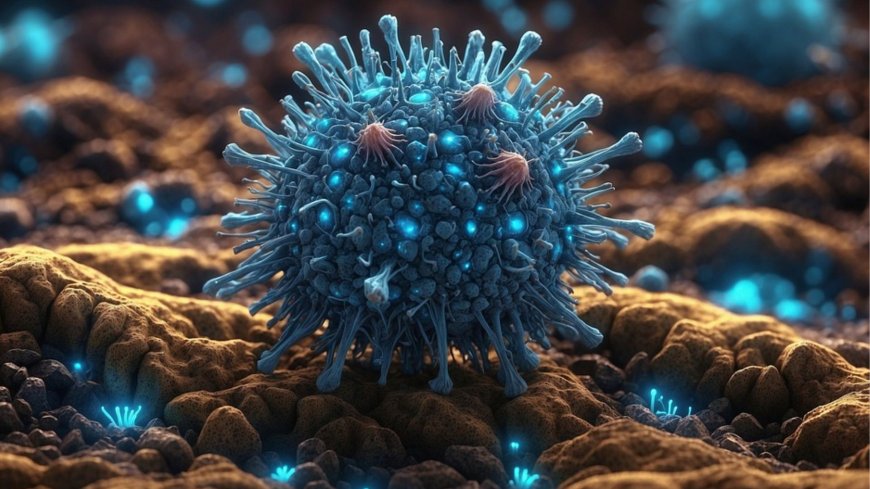
Antibiotic resistance occurs when bacteria evolve to withstand the effects of drugs that were once effective at killing them. This resistance makes it difficult or impossible to treat common infections with standard antibiotics. As more bacteria become resistant, the options for effective treatment shrink, leaving people vulnerable to infections that were previously manageable. Resistant bacteria can spread rapidly, creating a global health crisis that impacts every country.
Complications in Treating Common Diseases
What might begin as a simple infection, such as a respiratory infection or even a cold, can become far more difficult and dangerous to treat if antibiotic resistance develops. Infections that were once treatable with antibiotics may require longer courses of treatment or even hospitalization. Conditions like pneumonia or urinary tract infections can become life-threatening when the bacteria causing them become resistant to common antibiotics.
Increased Side Effects and Health Risks
The misuse of antibiotics can also lead to an imbalance in the body's natural microbiome. When antibiotics are taken unnecessarily or for extended periods, they not only target harmful bacteria but also kill beneficial bacteria in the body. This can result in digestive problems, weakened immunity, and other long-term health issues. Moreover, overuse of antibiotics increases the likelihood of adverse reactions, such as allergic reactions or the development of other infections, such as C. difficile (Clostridium difficile) in the intestines, which can cause severe complications.
In essence, antibiotic misuse doesn't just create immediate health risks but also puts humanity at risk by threatening our ability to treat common infections. The danger lies not only in the immediate effects but in the long-term consequences for public health worldwide.
Antibiotic Resistance: What is it and How Does it Develop?
Antibiotic resistance is a situation in which bacteria develop the ability to resist the effects of drugs that once killed them or inhibited their growth. This resistance means that the antibiotics prescribed to treat infections become ineffective, making it more difficult to treat common bacterial diseases. It is a natural process that can be accelerated by the misuse and overuse of antibiotics, especially when they are used unnecessarily or incorrectly.
How Does Antibiotic Resistance Develop?
Bacteria evolve constantly, and through natural processes, some bacteria may possess genetic mutations that allow them to survive exposure to antibiotics. These mutations may enable the bacteria to resist the actions of the antibiotics, and when the bacteria reproduce, these resistant traits are passed down to future generations.
Antibiotic resistance typically occurs in the following ways:
1. Overuse of Antibiotics: When antibiotics are used unnecessarily, such as for viral infections (e.g., the common cold), they provide an opportunity for bacteria to adapt. Overuse in both human medicine and agriculture accelerates this process.
2. Improper Use of Antibiotics: Taking antibiotics without a prescription, not completing the prescribed course, or taking the wrong type of antibiotic for the infection, allows bacteria to survive and develop resistance.
3. Transmission of Resistant Bacteria: Resistant bacteria can spread from person to person or through contaminated food or water, leading to widespread resistance across populations and even across countries.
Impact of Antibiotic Resistance
Antibiotic resistance poses a serious threat to global health by making it increasingly difficult to treat infections that were once easily manageable. As bacteria become resistant to commonly used antibiotics, the consequences are far-reaching, affecting both individual health and the broader healthcare system. Here are some of the critical risks posed by antibiotic resistance:
1. Increased Difficulty in Fighting Life-Threatening Infections
One of the most concerning effects of antibiotic resistance is its impact on the ability to treat life-threatening infections. Conditions that were once easily treatable with antibiotics, such as pneumonia, kidney infections, and urinary tract infections, can become much harder to manage. Infections that would typically clear up within a few days of antibiotic treatment may persist for longer periods, requiring more intensive and prolonged treatment, or in some cases, leading to complications that can result in death.
As antibiotic resistance continues to spread, doctors may find themselves without effective treatment options, which could lead to an increase in mortality rates from diseases that were once easily controlled.
2. Problems in Preventing Post-Surgery Infections
Another significant risk of antibiotic resistance is its impact on surgical procedures. Surgeons often rely on antibiotics to prevent infections after surgeries, but with the rise of resistant bacteria, post-surgical infections are becoming more difficult to prevent. This can lead to prolonged hospital stays, complications, or even life-threatening scenarios. Procedures that were previously considered low-risk, such as dental surgeries, cesarean sections, or joint replacements, now carry an increased risk of infection.
The inability to effectively treat infections in surgical patients can also lead to long-term health issues, including the need for additional surgeries, organ damage, or permanent disability.
3. Emergence of Stronger, More Dangerous Bacteria
As bacteria evolve to resist the effects of antibiotics, they may also develop new mechanisms to become even more dangerous. Some resistant bacteria have acquired the ability to become more virulent or to infect more areas of the body, making them harder to treat and control. The rise of superbugs, or bacteria resistant to multiple antibiotics, is particularly alarming. Infections caused by superbugs can spread rapidly, and their treatment options are limited, often requiring the use of more toxic and less effective drugs.
The development of superbugs could make common infections untreatable, increasing the burden on healthcare systems globally.
Global Problem and Solutions
Antibiotic resistance has emerged as a severe global health threat, and its spread poses a significant challenge to the treatment of bacterial infections worldwide. According to the World Health Organization (WHO), if this problem is not addressed soon, it could result in nearly 10 million deaths per year by 2050. This would make antibiotic resistance a leading cause of death, surpassing cancer. The rise of resistant bacteria has transformed what was once a manageable problem into a systemic issue, requiring coordinated global action.
The Global Nature of Antibiotic Resistance
Antibiotic resistance occurs when bacteria evolve in response to the overuse and misuse of antibiotics, rendering common treatments ineffective. This crisis is not confined to one region or country; it is a worldwide phenomenon, affecting both developed and developing nations alike. The misuse of antibiotics, whether in healthcare, agriculture, or veterinary medicine, has led to the acceleration of resistance. The growing number of multidrug-resistant (MDR) bacteria makes it increasingly difficult to treat infections that were once easily managed with antibiotics.
Global Impact and Unintended Consequences
The misuse of antibiotics has had profound consequences in various countries. Below are a few examples of how antibiotic misuse has led to unintended health crises:
1. Bangladesh:
In Bangladesh, the widespread use of antibiotics without prescriptions has led to an increase in antibiotic-resistant diseases, such as drug-resistant pneumonia and dengue fever. Many individuals take antibiotics without consulting a healthcare provider, or they fail to complete prescribed courses, which fosters resistance. As a result, the treatment of common infections has become more difficult, and healthcare providers are struggling to manage cases effectively.
2. India:
India is facing a particularly severe challenge due to the overuse and misuse of antibiotics. The country has experienced a rise in drug-resistant tuberculosis (TB), with bacteria no longer responding to the first-line treatments. The lack of regulation in both healthcare and agricultural sectors has led to the rapid spread of resistant bacteria, complicating the treatment of TB and other common infections. Consequently, many patients experience prolonged illness and even death due to ineffective treatments.
3. United Kingdom and European Nations:
In the UK and other European countries, antibiotic resistance has made it harder to treat respiratory infections, kidney infections, and pneumonia. As a result, some patients undergoing surgery face an increased risk of infection that cannot be treated effectively due to resistance. Multidrug-resistant infections, particularly those that develop in hospitals, have also led to a rise in complications and death rates among hospitalized patients.
4. Southeast Asia and Africa:
In regions like Southeast Asia and sub-Saharan Africa, the challenge of antibiotic resistance is exacerbated by limited healthcare infrastructure. Infections such as malaria and dengue fever are becoming harder to treat due to resistant bacteria, leading to higher mortality rates, especially in children. Furthermore, the availability of antibiotics over-the-counter, without prescriptions, has contributed to the misuse of these drugs and the spread of resistant infections.
5. United States:
In the United States, the overuse of antibiotics in hospitals and in the treatment of conditions such as sinus infections, ear infections, and flu has led to the rise of resistant strains of staphylococcus (MRSA) and other bacteria. Nosocomial (hospital-acquired) infections, caused by resistant bacteria, have become a serious problem in healthcare facilities, resulting in longer hospital stays, more intensive treatments, and higher death rates.
Global Coordination is Essential
Antibiotic resistance is no longer just a local issue—it is a global health crisis. The transboundary nature of resistance means that resistant bacteria can travel across borders, making international coordination essential. Countries must work together to establish shared protocols for antibiotic prescription, monitor antibiotic use, and enforce stronger regulations on their sale.
The World Health Organization has called for global cooperation to tackle antibiotic resistance, including:
- Reducing antibiotic misuse in both healthcare and agriculture
- Improving infection control measures in hospitals
- Enhancing diagnostics to ensure antibiotics are only prescribed when necessary
- Investing in the development of new antibiotics and alternative treatments
As antibiotic resistance spreads, it becomes increasingly difficult to treat infections effectively. The actions we take today will determine the future of antibiotic effectiveness. If left unchecked, we risk returning to a time when simple infections could once again become deadly, a reality that humanity must avoid at all costs.
Measures to Combat Antibiotic Misuse
Combating the misuse of antibiotics is crucial to curbing the growing problem of antibiotic resistance. Various proactive steps can be implemented by governments, healthcare professionals, and communities to minimize antibiotic overuse and ensure these life-saving medications remain effective for future generations. Below are some key measures that can be taken to address this issue:
1. Government Policies and Enforcement
Governments play a pivotal role in regulating antibiotic use. Strong policy frameworks need to be established that govern the sale and distribution of antibiotics. This includes:
- Strict regulations on over-the-counter sales of antibiotics, ensuring they can only be dispensed with a prescription.
- Enforcement of laws that penalize inappropriate antibiotic use in agriculture and healthcare settings, especially when antibiotics are administered for non-bacterial infections or when not required.
- Monitoring and controlling antibiotic use in both human healthcare and livestock farming. In many regions, antibiotics are used in animals for growth promotion, contributing to the development of resistant bacteria that can be transmitted to humans. Policies must be enacted to regulate and limit such practices.
2. Training and Awareness Campaigns for Healthcare Professionals and the Public
Increased education and training are essential in promoting responsible antibiotic use. This includes:
- Ongoing education programs for doctors, nurses, and other healthcare professionals on proper antibiotic prescribing practices. Healthcare providers must be trained to identify when antibiotics are truly necessary and to educate patients on the dangers of misuse.
- Awareness campaigns aimed at the general public about the risks of taking antibiotics without prescriptions or not completing a full course of treatment. People must be informed that antibiotics are not effective against viral infections like the flu or the common cold. These campaigns can be broadcast through various media, community outreach programs, and online platforms.
3. Standardized Guidelines for Antibiotic Use in Healthcare
Establishing and enforcing clear, evidence-based guidelines for antibiotic prescribing within healthcare settings is critical to ensure antibiotics are used only when necessary. These guidelines should include:
- Antibiotic stewardship programs that promote the appropriate use of antibiotics across hospitals and clinics. These programs ensure that antibiotics are prescribed only when necessary and at the correct dosages and durations.
- Treatment protocols for common infections should be regularly updated to reflect the latest research on bacterial resistance patterns, ensuring that doctors are prescribing the most effective and least harmful treatments.
- Collaborative efforts between healthcare professionals, scientists, and regulatory bodies to develop comprehensive strategies for monitoring and reducing unnecessary antibiotic prescriptions.
4. International Cooperation and Data Sharing
Since antibiotic resistance is a global issue, international cooperation is essential in tackling the problem. Countries should collaborate on:
- Global surveillance systems to monitor antibiotic use and resistance patterns worldwide.
- Data sharing initiatives to track the spread of resistant bacteria across borders and to implement effective containment strategies.
- Development of new antibiotics and alternatives, encouraging global research into new medicines, vaccines, and treatments to combat resistant infections.
5. Incentivizing Research and Development
One of the underlying factors contributing to the rise of antibiotic resistance is the lack of new antibiotics being developed. The pharmaceutical industry has been slow to develop new antibiotics due to economic and regulatory challenges. Governments and international organizations should create incentives for research and development of new antibiotics, including:
- Funding for antibiotic research to discover new classes of antibiotics.
- Partnerships between private and public sectors to accelerate the development of new medications that can target resistant bacteria.
6. Improved Infection Control Practices
Strengthening infection control measures in healthcare settings, such as hospitals and clinics, is crucial in reducing the spread of resistant bacteria. This includes:
- Strict hygiene protocols to prevent the transmission of infections, such as handwashing, sterilizing medical equipment, and isolating patients with resistant infections.
- Enhanced patient monitoring to ensure that infections are diagnosed early and that the appropriate treatment is initiated promptly, minimizing the need for unnecessary antibiotic use.
Conclusion
Antibiotics have undeniably revolutionized modern medicine, saving countless lives by effectively treating bacterial infections. However, the misuse and overuse of these critical drugs have given rise to antibiotic resistance, a growing global health crisis that threatens to undermine medical advancements. Antibiotic resistance not only complicates the treatment of common infections but also endangers patients undergoing surgeries, disrupts healthcare systems, and exacerbates mortality rates worldwide.
Addressing this issue requires urgent, coordinated efforts across governments, healthcare systems, and communities. Measures such as stringent regulations on antibiotic use, public awareness campaigns, and international collaboration are essential to mitigate the misuse of antibiotics. Additionally, incentivizing research into new antibiotics and improving infection control practices will play a crucial role in safeguarding the effectiveness of these life-saving medications.
If left unchecked, antibiotic resistance could mark a return to an era where minor infections become life-threatening, underscoring the need for immediate and sustained global action. The future of public health depends on our collective responsibility to use antibiotics wisely and preserve their efficacy for generations to come.
What's Your Reaction?